Condition: Stuttering
Definition:
Stuttering, the most common fluency disorder, is an interruption in the flow of speaking characterized by specific types of disfluencies, including
- repetitions of sounds, syllables, and monosyllabic words (e.g., “Look at the b-b-baby,” “Let’s go out-out-out”);
- prolongations of consonants when it isn’t for emphasis (e.g., “Ssssssssometimes we stay home”); and
- blocks (i.e., inaudible or silent fixation or inability to initiate sounds).
These disfluencies can affect the rate and rhythm of speech and may be accompanied by
- negative reactions to speaking;
- avoidance behaviors (i.e., avoidance of sounds, words, people, or situations that involve speaking);
- escape behaviors, such as secondary mannerisms (e.g., eye blinking and head nodding or other movements of the extremities, body, or face); and
- physical tension.
Children and adults who stutter also frequently experience psychological, emotional, social, and functional consequences from their stuttering, including social anxiety, a sense of loss of control, and negative thoughts or feelings about themselves or about communication (Boyle, 2015; Craig & Tran, 2014; Iverach et al., 2016; Iverach & Rapee, 2014).
Stuttering typically has its origins in childhood. Approximately 95% of children who stutter start to do so before the age of 4 years, and the average age of onset is approximately 33 months. Onset may be progressive or sudden. Some children go through a disfluent period of speaking. It is also not unusual for disfluencies to be apparent and then seem to go away for a period of weeks or months only to return again. Approximately 88%–91% of these children will recover spontaneously with or without intervention (Yairi & Ambrose, 2013).
Stuttering can co-occur with other disorders (Briley & Ellis, 2018), such as
- attention-deficit/hyperactivity disorder (Donaher & Richels, 2012; Lee et al., 2017),
- autism spectrum disorder (Briley & Ellis, 2018),
- intellectual disability (Healey et al., 2005),
- language or learning disability (Ntourou et al., 2011),
- seizure disorders (Briley & Ellis, 2018),
- social anxiety disorder (Brundage et al., 2017; Craig & Tran, 2014; Iverach et al., 2018),
- speech sound disorders (St. Louis & Hinzman, 1988; Wolk et al., 1993), and
- other developmental disorders (Briley & Ellis, 2018).
DSM-5 Diagnostic Criteria for "Childhood Onset Fluency Disorder":
Criterion A
Disturbances in the normal fluency (i.e. – dysfluencies) and time patterning of speech that are inappropriate for the individual’s age and language skills, persist over time, and are characterized by frequent and marked occurrences of at least 1 of the following:
- Sound and syllable repetitions
- Sound prolongations of consonants as well as vowels
- Broken words (e.g. – pauses within a word)
- Audible or silent blocking (filled or unfilled pauses in speech)
- Circumlocutions (word substitutions to avoid problematic words)
- Words produced with an excess of physical tension
- Monosyllabic whole-word repetitions (e.g. – “I-I-I am fine”)
Other Diagnostic Features
Interestingly, the dysfluencies from stuttering are usually absent during oral reading, singing, or talking to inanimate objects or to pets. The deficits are most severe when there is a special pressure to communicate or a stressful environment.
Criterion B
The disturbance causes anxiety about speaking or limitations ineffective communication, social participation, or academic or occupational performance, individually or in any combination.
Criterion C
The onset of symptoms is in the early developmental period. (Adults are diagnosed as adult-onset fluency disorder).
Criterion D
The disturbance is not attributable to a speech-motor or sensory deficit, disfluency associated with neurological insult (e.g. – stroke, tumour, trauma), or another medical condition and is not better explained by another mental disorder.
Evaluation:
Individuals are referred to a speech-language pathologist (SLP) for a comprehensive assessment when disfluencies are noted and when one or more of the factors listed below are observed along with the disfluencies.
This list is not exhaustive, and not all factors need to be present for a referral to an SLP (e.g., Guitar, 2019; Yaruss et al., 1998).
- There is a family history of stuttering or cluttering.
- There is parent/individual concern.
- The person exhibits negative reactions (e.g., affective, behavioral, or cognitive reactions) to their disfluency.
- The person is experiencing negative reactions from others (e.g., peers, classmates, coworkers, family members).
- The person exhibits physical tension or secondary behaviors (e.g., eye blinking, head nodding) associated with the disfluency.
- The person is having difficulty communicating messages in an efficient, effective manner.
- Other speech or language concerns are also present.
Consistent with the World Health Organization’s (WHO) International Classification of Functioning, Disability and Health (ICF) framework (ASHA, 2016a; Coleman & Yaruss, 2014; Vanryckeghem & Kawai, 2015; WHO, 2001; Yaruss, 2007; Yaruss & Quesal, 2004, 2006), a comprehensive fluency assessment is conducted to identify and describe
- impairments in body structure and function, including frequency and severity of disfluencies, presence of physical concomitant behaviors and learned avoidance behaviors, and presence of tension and effort while communicating;
- comorbid deficits or conditions, such as speech sound disorders and language disorders;
- limitations in activity and participation, including functional communication and interpersonal interactions at home, in social settings, at school, or at work;
- contextual (environmental and personal) factors that serve as barriers to or facilitators of successful communication and life participation; and
- the impact of communication impairments on quality of life of the individual.
A comprehensive fluency assessment typically includes the following:
- Relevant case history (as appropriate for age)
- Consultation with family members, educators, and other professionals regarding fluency variability (when disfluencies are noticed most and least) and the impact of disfluency.
- Real-time analysis or analysis based on an audiovisual recorded speech sample demonstrating representative disfluencies beyond the clinic setting.
- Review of previous fluency evaluations and educational records.
- Assessment of speech fluency (e.g., frequency, type, and duration of disfluencies), speech rate, speech intelligibility, and the presence of secondary behaviors in a variety of speaking tasks (e.g., conversational and narrative contexts).
- Assessment of awareness in young children of disfluencies and difficulty in speaking.
- Stimulability testing (e.g., person is asked to increase pausing and/or decrease speech rate in some other way)—a reduction of overall speech rate typically helps in reducing cluttering symptoms.
- Assessment of the impact of stuttering or cluttering—including assessment of the emotional, cognitive, and attitudinal impact of disfluency.
- Assessment of other communication dimensions, including speech sound production, receptive and expressive language, pragmatic language, voice, hearing, and oral–motor function/structure.
- Determination of individual strengths and coping strategies.
Source: https://www.asha.org/practice-portal/clinical-topics/fluency-disorders/#collapse_5
Our Resources for Evaluating Stuttering:
The Whole Child Approach to Evaluating and Treating Stuttering – Webinar Recording
This one-hour webinar recording will show you how to consider the whole child while evaluating and treating stuttering in children.
Overview of How to do a Fluency Evaluation
Need the quick version? This shorter video will give you the overview of how to conduct a fluency evaluation.
Suggested Goals:
The results of the assessment process should help guide what you will target in therapy for a child who stutters. Here are some goals that may need to be addressed in children with autism. You can click on one of the goals below to learn more. Or, scroll down to the therapy section for more in-depth resources and support for treating this condition.
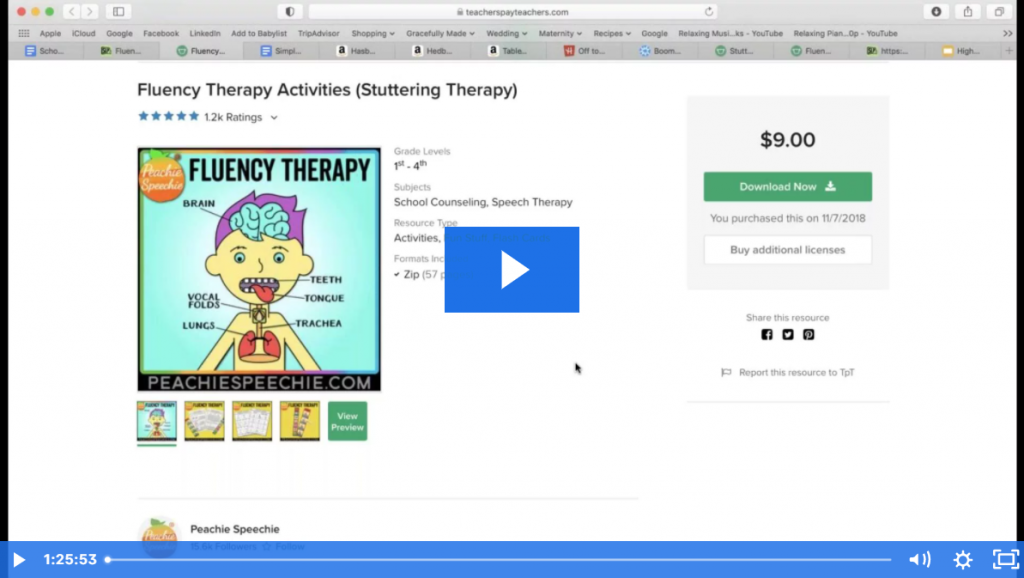
Therapy:
Here are some more resources and information that may help you when it comes to treating this condition.
Treatment of Stuttering in Middle and High School Students – Webinar Recording
Hour-long presentation covering therapy ideas and suggestions when working with children from grades 6-12.
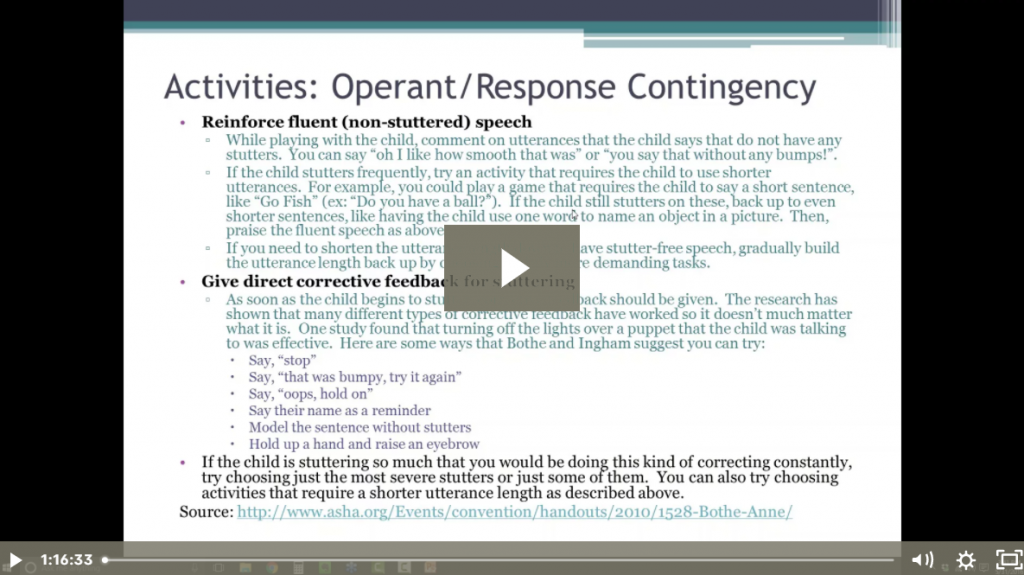
The Whole Child Approach to Evaluating and Treating Stuttering – Webinar Recording
This one-hour webinar recording will show you how to consider the whole child while evaluating and treating stuttering in children.
Stuttering/Fluency Therapy Activities – Webinar Recording
Another hour-long presentation packed full of stuttering/fluency activity ideas for all ages.
Direct vs. Indirect Therapy for Preschool Stuttering
This short video explains when you should do direct therapy vs. indirect therapy for preschool stuttering. This video also discusses the “red flags” that indicate that developmental stuttering may become persistent stuttering.
Using the 4-7-8 Breathing Technique to Ease Tension with Stuttering
This quick breathing exercise is great for children who have tension and/or anxiety that is contributing to their stuttering.
Fluency/Stuttering Therapy for Middle Schoolers
This short video covers what to target in stuttering therapy with middle schoolers (grades 5-8).
Acquired Stuttering vs. Developmental Stuttering
Learn the difference between developmental stuttering (aka child onset stuttering) and neurogenic or acquired stuttering (aka adult onset stuttering).
Onboarding a New Student Who Stutters
This short video answers a question from a member who received a transfer student who qualified for services based on a stutter.
Generalizing Fluency Strategies Outside the Therapy Room
A short video with extra ideas and tips for those children who can use the strategies during therapy but are struggling to generalize them outside the therapy room.
Overview of How Breathing Exercises Work into Fluency Therapy
This short video will explain how breathing exercises can be an important part of fluency therapy.
What is Language Formulation Dysfluency?
Have you ever heard the term language formulation dysfluency? Here’s what it’s all about.
Didn’t Find What You’re Looking For?
We’re constantly working on adding new features and topics to this membership site. If you don’t find what you’re looking for by using the search bar at the top of the page, please use the button below to request new features or topics to be added!