Condition: Traumatic Brain Injury (TBI)
Jump To:
Severity Evaluation Therapy Suggested Goals
Definition:
Traumatic brain injury (TBI) is a form of nondegenerative acquired brain injury resulting from a bump, blow, or jolt to the head (or body) or a penetrating head injury that disrupts normal brain function (Centers for Disease Control and Prevention [CDC], 2015).
TBI can cause brain damage that is focal (e.g., gunshot wound), diffuse (e.g., shaken baby syndrome), or both. Symptoms can vary depending on site of lesion, extent of damage to the brain, and the child’s age or stage of development.
The functional impact of TBI in children can be different than in adults—deficits may not be immediately apparent because the pediatric brain is still developing. TBI in children is a chronic disease process rather than a one-time event, because symptoms may change and unfold over time (DePompei & Tyler, in press; Masel & DeWitt, 2010).
Source: https://www.asha.org/practice-portal/clinical-topics/pediatric-traumatic-brain-injury/
Severity:
TBI can result from a primary injury or a secondary injury (see common classifications of TBI for more details). Severity of TBI may be categorized as mild, moderate, or severe, based on the extent and nature of injury, duration of loss of consciousness, posttraumatic amnesia (PTA; loss of memory for events immediately following injury), and severity of confusion at initial assessment during the acute phase of injury (Diagnostic and Statistical Manual of Mental Disorders, 5th ed. [DSM-5; American Psychiatric Association, 2013]; CDC, 2015).
- Mild TBI (mTBI) — loss of consciousness for less than 30 minutes, an initial Glasgow Coma Scale (GCS) or Pediatric GCS of 13–15 after 30 minutes of injury onset, and PTA for not greater than 24 hours (CDC, 2015; McCrory et al., 2013; Ontario Neurotrauma Foundation, 2013).
- Uncomplicated — mTBI where there are no overt neuroimaging findings.
- Complicated — mTBI where there are intracranial abnormalities (e.g., bruising or a collection of blood in the brain) seen on CT scan or MRI.
- Moderate TBI — loss of consciousness and/or PTA for 1–24 hours and a GCS of 9–12 (CDC, 2015).
- Severe TBI — loss of consciousness for more than 24 hours and PTA for more than 7 days with a GCS of 3–8 (CDC, 2015).
Concussion, a form of mTBI, is an injury to the brain characterized by the physical and cognitive sequelae of TBI. Concussion typically occurs as a result of a blow, bump, or jolt to the head, face, neck, or body that may or may not involve loss of consciousness (McCrory et al., 2013). Concussion has received more attention in recent years, particularly with respect to sports injuries.
Source: https://www.asha.org/practice-portal/clinical-topics/pediatric-traumatic-brain-injury/
Evaluation:
Children and adolescents with TBI are a heterogeneous group with varied and complex sequelae that can change over time. Assessment of children with TBI takes into account the child’s behaviors, strengths, and needs over the course of development and rehabilitation, including school and community re-entry. For children in particular, it is helpful to focus assessment on areas critical to learning and school success. Assessment requires ongoing collaboration with the family and medical, surgical, rehabilitation, and educational professionals. Findings from the speech-language and audiologic assessments are analyzed in the context of findings from other professionals on the team. See ASHA’s web page on Interprofessional Education/Interprofessional Practice (IPE/IPP).
Source: https://www.asha.org/practice-portal/clinical-topics/pediatric-traumatic-brain-injury/#collapse_5
Check out our resources about evaluation of pediatric traumatic brain injury:
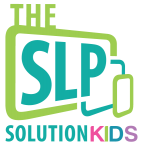
Pediatric TBI Evaluation and Treatment – Webinar Recording
A full, hour-long presentation that covers strategies for evaluating and treating children with traumatic brain injuries.
Suggested Goals:
Goals for children with TBI should be tailored to the specific impairments that those children experience. Here are links to some areas that are commonly disordered in children with TBI:
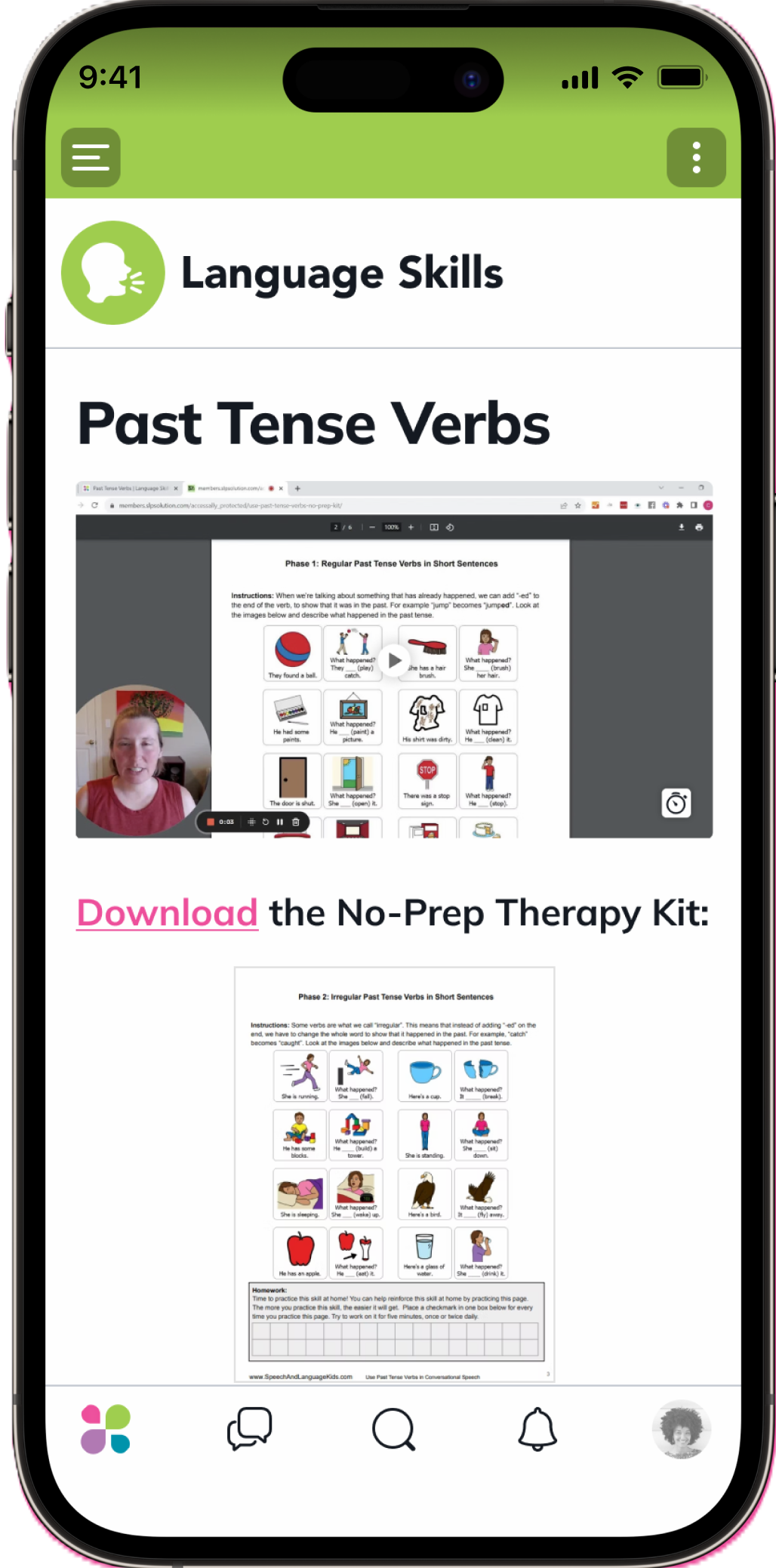
Therapy:
Here are some more resources and information that may help you when it comes to treating this condition.
Pediatric TBI Evaluation and Treatment – Webinar Recording
A full, hour-long presentation that covers strategies for evaluating and treating children with traumatic brain injuries.
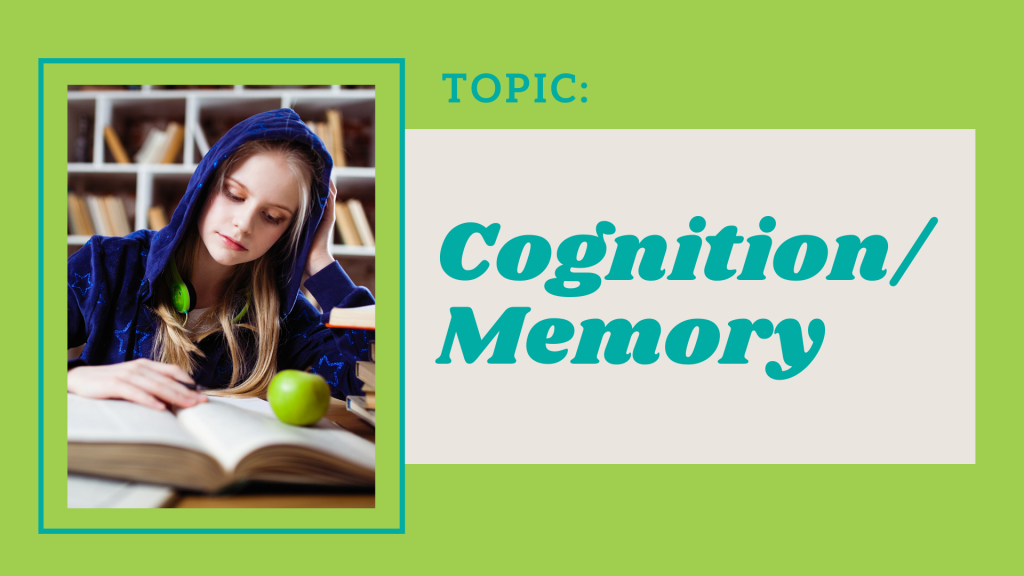
A quick video with tips for working with a child who has experienced acquired dysgraphia after a TBI.
Didn’t Find What You’re Looking For?
We’re constantly working on adding new features and topics to this membership site. If you don’t find what you’re looking for by using the search bar at the top of the page, please use the button below to request new features or topics to be added!