Condition: Oral Motor and Proprioception Concerns
Definition:
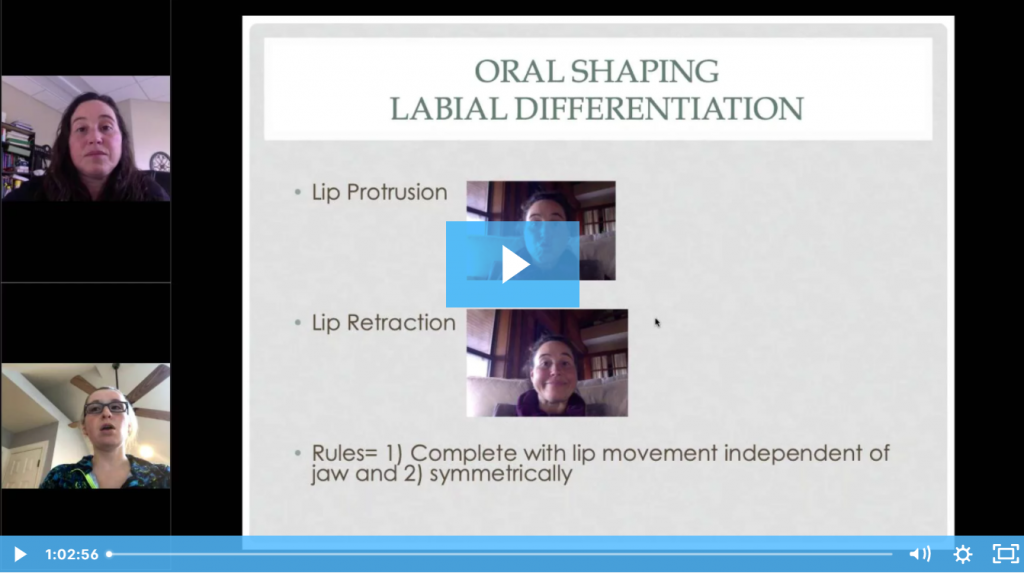
Many of our clients in therapy for speech sounds have difficulty using their articulators (tongue, jaw, lips, etc.) appropriately to create the sounds. For these children, it’s not enough to simply teach them what it should sound like. We must help them learn how to move their articulators to produce it as well.
Different Types of Oral Motor Concerns:
- Motor Speech Disorders: Disorders where the motor planning of speech is impaired, such as with childhood apraxia of speech.
- Orofacial Myofunctional Disorders: Patterns involving oral and orofacial musculature that interfere with normal growth, development, or function of orofacial structures, or call attention to themselves (Source). These types of disorders can affect speech as well as swallowing/feeding.
- Oral Structural Problems: Issues with the physical structures used to produce speech, such as cleft lip/palate or tongue tie. Physical limitations due to these conditions can impact the child’s ability to produce certain speech sounds.
- Oral Awareness/Proprioception Concerns: Child has low awareness of his/her articulators and/or isn’t able to feel or understand where they are and how they are being used. This is not a diagnosis but can occur in children with diagnoses such as motor speech disorders, orofacial myofuncitonal disorders, or articulation disorder/delays.
- Oral Coordination Concerns: Child has difficulty coordinating the movements of the articulators to get them into the proper position for speech sound production. This is not a diagnosis but can occur in children with diagnoses such as motor speech disorders, orofacial myofuncitonal disorders, or articulation disorder/delays.
But Wait...Aren't Non-Speech Oral Motor Exercises (NSOMEs) Bad??
Great question! We’re so glad you asked! 😉
We get this question a lot when we start to talk about oral awareness, oral proprioception, and oral coordination. Here is our official stance on this although there are many people with many strong opinions on this topic so you may hear different advice if you look elsewhere. Here is our understanding based on the current research and our clinical expertise and experience. Please use your professional judgement and do your own reviews of the research when considering approaches to use with your clients.
What Are Non-Speech Oral Motor Exercises (NSOMEs)?
According to ASHA: Nonspeech oral–motor therapy involves the use of oral-motor training prior to teaching sounds or as a supplement to speech sound instruction. The rationale behind this approach is that (a) immature or deficient oral-motor control or strength may be causing poor articulation and (b) it is necessary to teach control of the articulators before working on correct production of sounds. (Source)
Examples: So non-speech oral motor exercises would be movements that a child does with his/her articulators that do not involve speech. And these movements are done repetitively, just like doing reps of an exercise at the gym. Imagine things like “wagging the tongue back and forth” or “pretending your tongue is a paint brush and paint the roof of your mouth from front to back”.
Are NSOMEs Bad?
Systematic research reviews have shown that there is “currently no strong evidence suggests that [non-speech oral motor treatments] NSOMTs are an effective treatment or an effective adjunctive treatment for children with developmental speech sound disorders” (Source)
That means… there is no evidence that using NSOMEs alone will improve speech sounds or that they are required for a child to be able to improve speech sound production.
So How is This Different?
What we’re suggesting here is not the same as NSOMEs. We are not suggesting that every child should be able to wag his tongue before speech therapy is conducted. We’re not suggesting that if you have a client wag his tongue 30 times per day, his speech sounds will improve.
What we’re talking about here is what to do if a child CAN’T put his articulators in the correct places or perform the correct movements to produce certain speech sounds. There are things you can do with the child to help them move their articulators into the correct positions to produce speech sounds.
How They're Different:
| Non-Speech Oral Motor Exercises | Oral Awareness, Proprioception, Coordination |
|---|---|
| Repetitive exercises that don’t involve speech sounds | Exercises used to help a child get his articulators into the correct positions for speech sound production |
| Used independently of working on speech sounds | Immediately followed by speech sound production as soon as the child is able to produce the sound |
Examples:
| Examples:
|
Developmental Norms:
When looking at oral motor skills in children, it is important that we look at their functional impact. It is not important whether a child can lift his tongue up and down if that child is able to produce all speech sounds correctly and has a functional, efficient swallow. However, if a child is having difficulties with speech sounds or swallowing, then those oral motor skills may need to be examined as they relate to the specific problem that the child is experiencing.
For this reason, we should always first examine functional skills like speech sounds and swallowing to identify if the child is having oral motor problems that impact him/her. Take a look at the norms below to see if a child is on track.
The following ages represent that ages by which each sound was mastered by 75% of children (based on two studies, see source below).
- 2-3 Years: /m/, /n/, /h/, /p/,
- 2-4 Years: /f/, “y”, /k/, /g/, /d/
- 2-8 Years: /w/, /b/, /t/,
- 3-4 Years: /s/, /r/
- 3-6 Years: /l/
- 3-8 Years: “ch”, “sh”
- 4-6 Years: /v/, voiceless “th”
- 4-7 Years: /z/, “zh”, “j”, voiced “th”
Check out the following excerpt from an interview with Diane Bahr on the Ages and Stages website. This information comes from her book about infant mouth development and is an amazing resource if you’re looking for more information and training.
Source: http://www.agesandstages.net/qadetail.php?id=40
Birth to 3-month period (pp. 46-48) a baby:
- Roots to find the breast and/or bottle (if the parents use paced bottle feeding, pp. 25-26)
- Is fed breast milk and/or formula
- Moves from reflexive suckling to long bursts of purposeful sucking (e.g., 20+ without a pause)
3 to 6-month period (pp. 47-51), a baby’s mouth continues to develop. The baby:
- Roots less
- Develops a three-dimensional suck (where the tip and sides of the tongue move upward giving the tongue a nice bowl shape, the lips are puckered, and the cheek and jaw muscles begin to do the work that the fat pads were previously doing). The fat pads in the cheeks usually go away during this period.
6 to 9-month period (pp. 202-205) babies:
- Open their mouths just enough for the spoon to enter
- Start using the upper lip to clear food from the spoon
- Can pick up pieces of food with the fist and pass food from one hand to the other
- Begin moving the jaw just enough to match the shape and size of the food in the mouth
- Use their lips and cheeks to hold food within the mouth
- Begin to move their tongues toward food placed on the gums
- Begin getting a couple more teeth with appropriate chewing and biting experiences
- Therefore the baby is ready for a number of foods between 6 and 8-months (pp. 182-183):
- Milled, blended, or well-mashed fruits and vegetables that are well-cooked with soft lumps and given from a spoon
- Wheat-free baby cereal, wheat-free soft cookies and crackers
- Cooked sticky rice
- Sips of water and very diluted fruit and vegetable juices in an open cup (held by an adult) or a straw cup in addition to breast milk and formula
Between 7 and 10-months, you can introduce (p. 183):
- Chopped cooked fruits and vegetables, including canned fruits but not citrus
- Soft cheese
- Mashed cooked beans and tofu
- Wheat and corn products
During the 9 to 12-month period (pp. 206-207), babies:
- Begin to hold and bang the spoon
- Begin to pick up small pieces of food with the thumb and fingers
- Can break off cookie and cracker pieces with their hands when cookies or crackers are held by their jaws
- Move the jaw in an increasingly mature manner to match the shape and size of the food
- Move food from the center of the tongue to the gums for chewing
- Can drink from a straw-cup or from an open cup (held by an adult) with consecutive swallows (i.e., swallow after swallow)
During the 9 to 12-month period (pp. 183-184) you can introduce:
- Soft, cut-up cooked and raw foods while slowly introducing citrus
- Cooked fruit and vegetable strips
- Soft, chopped meats (e.g., stewed meats)
- Casseroles with noodles, pasta, and rice
- Bread, toast, crackers, and dry cereal
- Eggs (yolks at 9 months, whites at 12 months)
- Soft cheese strips, cottage cheese, and baby yogurt
Feeding development continues through 24 months. By 24 months a child’s feeding skills are just about the same as yours and mine. The 12 to 24-month period is a time for the refinement of the feeding skills begun in the first year. You can find these and others specifics about the critical learning period for feeding (i.e., birth to 24-months) in my book (Chapters 2 and 6).
More Info: https://members.slpsolution.com/condition-feeding-swallowing-concerns/
Evaluation:
Evaluation for oral motor concerns will vary greatly depending on the type of oral motor concerns that are present. Some structural problems, such as cleft lip/palate or tongue tie, may need to be evaluated by a medical team. For other conditions, such as motor speech disorders or orofacial myofunctional disorders, you may need additional training and/or certification to properly diagnose.
If you are evaluating a child with suspected oral motor concerns, you will need to determine their impact on speech and/or swallowing to determine what course to take during therapy.
Here are some additional resources for evaluation of children with oral motor concerns:
Evaluation of Feeding & Swallowing Disorders – Webinar Recording
A one-hour webinar recording that shows you how to conduct a comprehensive evaluation of feeding and swallowing skills in children.
Suggested Goals:
The results of the assessment process should help guide what you will target in therapy for a child with this condition. Here are some goals that you may be addressing with this population. You can click on one of the goals below to learn more. Or, scroll down to the therapy section for more in-depth resources and support for treating this condition.
Therapy:
Here are some more resources and information that may help you when it comes to treating this condition.
Supplemental Materials:
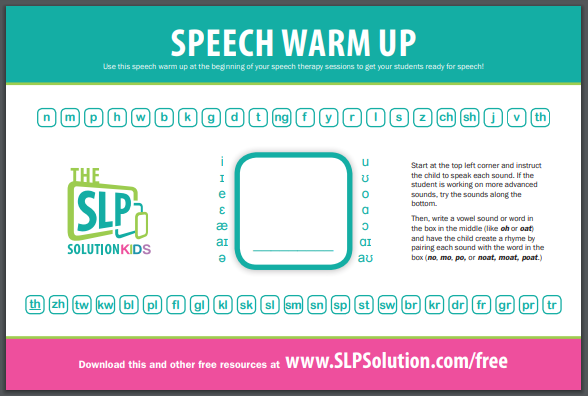
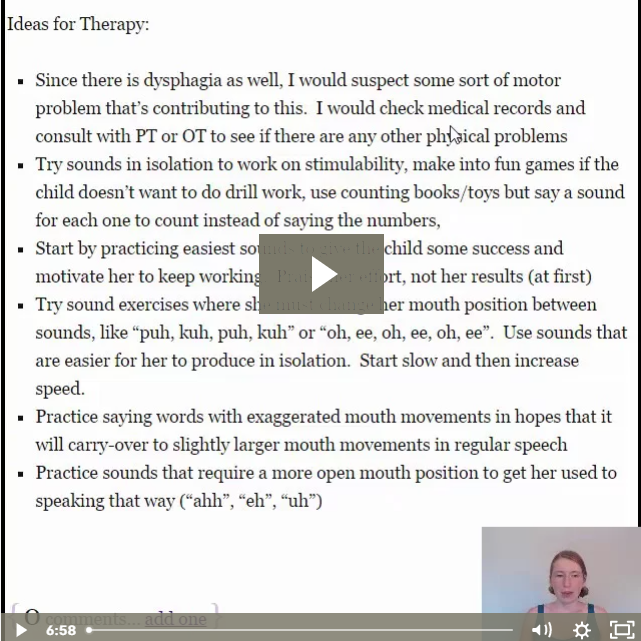
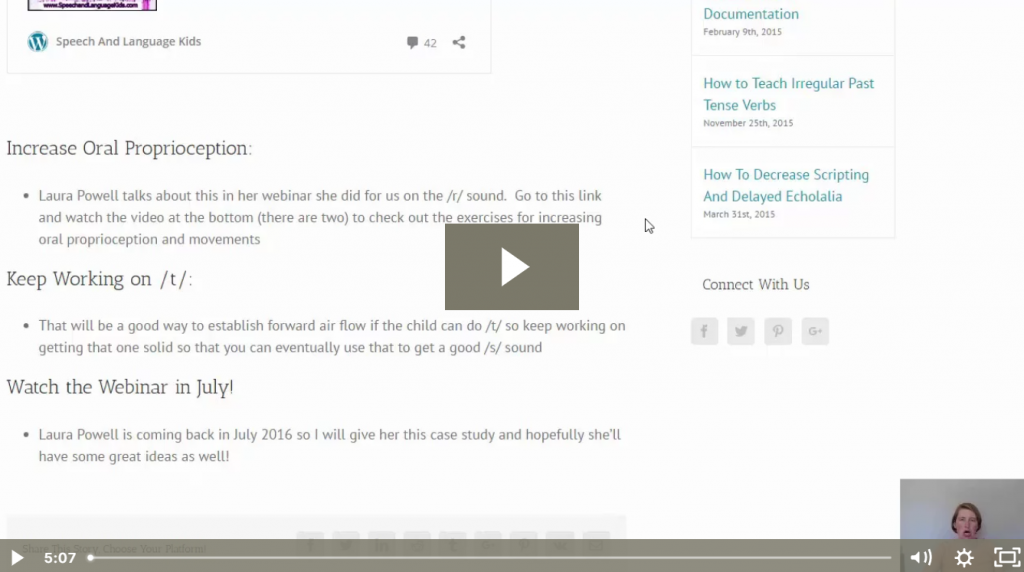
Training Videos:
Short videos that answer questions or review certain aspects of this condition:
How to Deal with Oral Structural Problems
Such as tongue tie, missing teeth, velopharyngeal insufficiency, etc.
Webinar Recordings:
Full, hour-long webinar presentations that go in depth on various topics.
Didn’t Find What You’re Looking For?
We’re constantly working on adding new features and topics to this membership site. If you don’t find what you’re looking for by using the search bar at the top of the page, please use the button below to request new features or topics to be added!